SpinopelvicMobilityApp app for iPhone and iPad
Developer: ORTHOPRACTIS.COM SINGLE MEMBER P.C.
First release : 22 Apr 2018
App size: 922 Kb
Evaluation of lateral radiographs in sitting and standing positions is of importance, especially in patient before total hip replacement surgery.The importance of understanding the hip spine relationship and the spinopelvic mobility has become increasingly recognised in recent years as a cause of hip instability with no previous known aetiology. Spinopelvic motion is a coordinated biomechanical relationship among acetabular anteversion, pelvic tilt, and lumbar lordosis. Hip instability due to spinopelvic mobility, specifically the move from standing to sitting, and the subsequent changes in pelvic orientation is associated with late dislocations in hip replacement surgery and revision. Awareness of this phenomenon by hip and spine surgeons and pre and post operative evaluation of the hips help guide the surgeon to the ideal location for cup implantation or to address the spine or hip pathology accordingly.
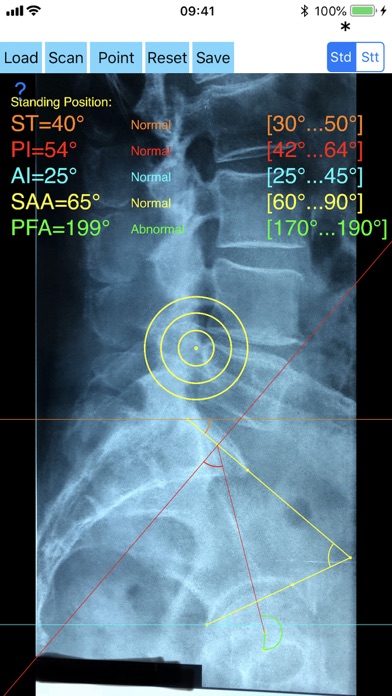
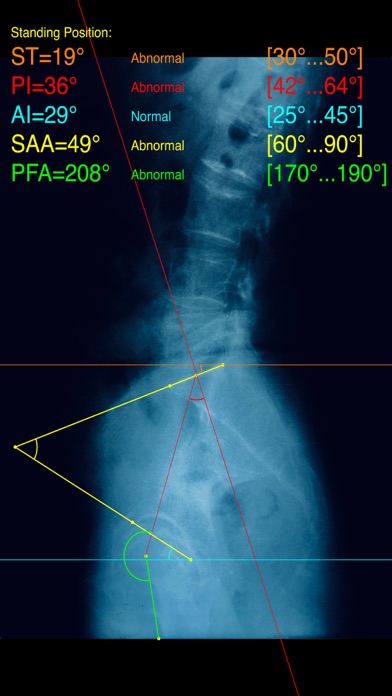
Radiographic measurement in lateral radiographs in sitting and standing positions of Pelvic incidence (PI), Sacral Tilt (ST), Ante-Inclination (AI), Sacro-acetabular angle (SAA) , Pelvic femoral Angle Angle (PFA) and Combined Sagittal Index (CSI) are of paramount importance. These data measured in standing and in sitting X-rays and compared both with normal reference data may help to evaluate and plan treatment strategies. In clinical settings measuring all these angles is cumbersome and App comes to help the surgeon to do the job without loosing time.
The Spinopelvic Mobility App is medical software aimed for orthopaedic surgeons, providing tools that allow doctors to:
-Securely import medical images directly from the camera or stored photos.
-By marking few points at the image of X-ray, the App calculates and offers a very convenient way to determine the most possibly accurate way at once, Combined Sagittal Index (CSI) ,Pelvic incidence (PI), Sacral Tilt (ST), Ante-Inclination (AI), Sacro-acetabular angle (SAA) , Pelvic femoral Angle Angle (PFA). According to measured parameters in standing and sitting lateral x- rays the app helps to identify patterns of spinopelvic mobility namely normal, hypermobile or three patterns of spinal imbalance: hips maintained in anterior tilt (stuck standing), hips held in posterior tilt (stuck sitting), or stiff hips or kyphotic sacrum and predict by CSI the possible direction of THA dislocation.
-Save the planned images, for later review or consultation.The measured values are compared by normal reference databases and also data are exported as txt file, ready to print or to input as cells to excel for research.
-The app allows choosing points in an in independent manner from order and thus it is easy to be learned and in case of wrong selection powerful undo feature is present.
All information received from the software output must be clinically reviewed regarding its plausibility before patient treatment! Spinopelvic Mobility App indicated for assisting healthcare professionals. Clinical judgment and experience are required to properly use the software.The software is not for primary image interpretation.
The build in feature of the app, allows results to be categorized may help decide what could be considered normal or pathologic.
This App is particular useful in clinical settings where you need a quick results without loosing time. Please see tutorial videos at the developer’s web site www.orthopractis.com
Reference
1.Lum ZC ,et al The Current Knowledge on Spinopelvic Mobility.J Arthroplasty. 2018 Jan;33(1):291-296.
2.Stefl M et all Spinopelvic mobility and acetabular component position for total hip arthroplasty. Bone Joint J. 2017 Jan;99-B(1 Supple A):37-45.
3.Tezuka T et al . Functional safe zone is superior to the Lewinnek safe zone for total hip arthroplasty: why the Lewinnek safe zone is not always predictive of stability. J Arthroplasty. 2019;34:3–8.
4. Heckmann N et al JBJS. 2018;100:1845–53.